by Lauren Agoratus, FVNJ, SPAN
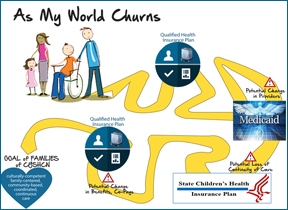
“Churn” in health care coverage means moving from health plan to health plan based on changes in eligibility. If families of children with special health care needs have a change in income or life circumstances, such as getting or losing a job and insurance that goes with it, they and their child may lose or gain eligibility for different health care plans. And, families whose income fluctuates during the year may lose or gain Medicaid or CHIP coverage. Such churn often causes disruptions in coverage, even if a child becomes eligible for a public program due to a decrease in income.
Good News/Bad News
The Commonwealth Fund discovered that the Affordable Care Act (ACA) will help families who have income or life changes by not dropping coverage completely. However, there is concern about what will happen when children with disabilities move back and forth between Qualified Health Plans (QHP) in the Marketplace and Medicaid or CHIP (State Children’s Health Insurance Program).
Possible Problems
There are serious implications for families moving either from a Marketplace plan to Medicaid/SCHIP or vice versa. These include:
- This affects a large number of families; 50% of families who have incomes that are below two times the poverty level will have at least one change in income which would switch them from Medicaid to the Marketplace or vice versa, even in states with no Medicaid expansion.
- When families change plans, they have to change to providers that participate in the new plan.
- Families moving from Marketplace to Medicaid plans or vice versa may lose family practitioners who were their usual source of care. This means that families may lose the primary doctor most familiar with their child’s special needs, affecting continuity of care.
Possible solutions
- Health plans could become multimarket plans to ensure smooth transition. However, benefit limits, copays, and deductibles will still change for families with a new plan.
- Using premium assistance, states can utilize Medicaid funding to help pay for private plan premiums, which will lead to a stable group of providers for families.
- States should have continuous enrollment for 12 months using annual enrollment which will ensure continuity of care for children with special needs.
- The Basic Health Program option could be used by states for consistency in benefit coverage. Note that 16 states have transition policies in place.
In summary, “In some cases, states establish general directives to plans to coordinate transfers; in others, state policies designate policies for issues such as transfer of medical records, maintenance of established patient–provider relationships for some time, and transition protocols for designated populations and conditions.” (Commonwealth Fund report)
Another good resource recently released by Community Catalyst is the “Churn Toolkit.” Several key points were found to affect churn reduction. These include consideration of:
- Application literacy level
- Language access to applications
- Conflicting information confusing to families
- Out-of-date family contact information
- Denial due to incomplete application
- Income/life changes
- Complexity of renewal process
Methods to mitigate these barriers are:
- Addressing health literacy will eliminate the single largest barrier to health care access.
- Applications in multiple languages will address underserved populations.
- Availability of both in-person and phone help will assist families with information integration.Using email, if available, could eliminate problems with returned mail due to incorrect addresses.
- “Express lane” eligibility determinations -- that is, using income data from another public program (e.g., WIC or food stamps) to determine eligibility for Medicaid or CHIP -- will reduce the need to provide income information for applications.
- Continuous eligibility for a set period of time will avoid the need to switch plans due to income or life changes.
- Express lane, continuous eligibility and administrative verification (i.e. using other sources) will help simplify renewal and aid in retention.
The ease of renewal is an important component of reducing churn by maintaining retention. Enroll America noted that the U.S. Department of Health and Human Services is proposing automatic enrollment for renewal (see “Renewal” under Resources.) Enroll America issued guidance to help families keep coverage through the Marketplace and automatic enrollment in states that have federally run Marketplaces. “These plans would give existing consumers a simple way to remain in the same plan next year unless they want to shop for another plan and choose to make changes.” Key factors include the provision of:
- consistent information and “…this information needs to be available by early September when new federal Navigator grantees are announced, so that Navigators can learn about renewals as part of their training and certification/recertification.”
- No action needed if no change to family information and “…HHS should build a renewal system that can accommodate enrollees whose situations are uncomplicated.”
- Minimize information required when reporting changes in family circumstances so that applicants need not submit a new application or resubmit information that is unchanged, such as verification of identity and citizenship.
- Clear messaging on deadlines, which will remind families how to keep continuous coverage, and reminders that people can enroll in Medicaid at anytime.
- Streamline transitions between the Marketplace and Medicaid by shortening the 9 page “model” form and by using prepopulated information fields and pretesting the forms with families.
Many emerging strategies are being proposed for states to reduce churn and aid in retention of families in health plans. Families can find help with children’s policy and family advocacy organizations (see “Finding State Resources” below.) Parents of children with special health care needs will benefit from these initiatives, resulting in consistent care.
Resources:
- Commonwealth Fund: Reducing churn
- Community Catalyst: Churn Toolkit-stabilizing coverage
- Community Catalyst: Finding state resources
- Community Catalyst: Policy approaches to churn
- Health & Human Services: Renewal – auto enrollment plans
- Enroll America -Policy recommendations for renewal
Comments